“We must embrace pain and burn it as fuel for our journey. ”
Cancer survivorship is often described as being disease-free, but not free of your disease. The truth is, going through cancer treatment is like swallowing a grenade. It may kill our enemy, but it kills a lot a bystanders too—damaging vital organs and causing a cascade of other health issues long after treatment has ended.
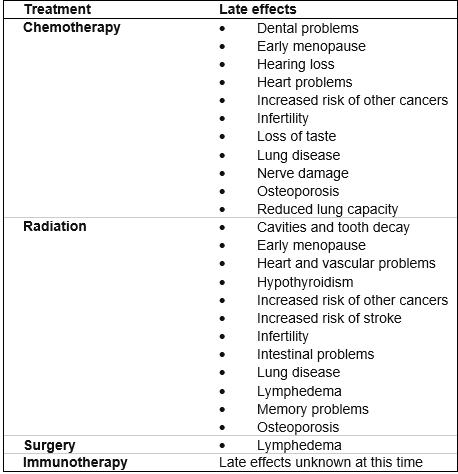
Chemotherapy and radiation destroy cancer cells. They also destroy normal, healthy cells in the process. Certain side effects can happen months or even years after your treatment. This may result from scarring to parts of the body or damage to internal organs.
Fatigue, difficulty concentrating (aka chemo brain), heart problems, reduced lung capacity, nerve problems, early menopause, muscle weakness, dental problems and secondary cancers are just some of the long-term side-effects related to cancer treatment. While the benefits of treatment typically far outweigh the risks, it’s important for cancer patients and their families to understand the long-term side-effects of cancer treatment.
I finished treatment for Stage 3 Hodgkin’s Lymphoma on August 9, 2018. Throughout my first year in remission, I’ve been dealing with crippling nausea, neuropathy, vision changes, hormonal and neurological issues, and ongoing heart problems.
Cancer treatment is often a trade-off, where you try to balance the risks of cancer-treatment for the chance to reach remission. Cancer patients are subjected to numerous scans, radiation, surgery and stem-cell transplants. Each treatment carries its own risks and while side effects from treatment are common, not everyone experiences them. However, long-term effects from treatment can show up months, even years later—long after treatment has ended. Some side effects are temporary, while others can last a lifetime.
While I don’t always talk about these long-term effects from treatment with friends and family, they are never far from mind. Every ache and pain or bodily change I notice is heavily scrutinized. Is this a sign of relapse or a latent effect from treatment?
Even when I’ve had excellent check-ups and scans that show no evidence of disease, it’s hard to shake the feeling that I’m living on borrowed time. Even when my outward appearance may show signs of health and vitality, internally it’s often a different story.
Whether it’s dealing with the crippling fear and anxiety of a potential relapse or physical symptoms like neuropathy and heart abnormalities, it’s hard to go a day without being reminded of the long-term effects of my treatment.
This reality hit me hard last weekend when I was hospitalized for possible pneumonia following a family vacation. My entire family came down with a cold. I was the last to get it, yet my immunocompromised body was unable to fight it off at home. Just four weeks earlier I was active, surprising myself and many by being able to play in my college alumni volleyball game. Suddenly, I found myself back in the ER, with a fever of 102.3, shaking from extreme chills and surrounded by an army of concerned doctors running every imaginable test to find out what was wrong. I ended up staying the entire weekend at the hospital.
It was hard at times to fight back the tears during my recent hospitalization. As I laid in my hospital bed, my body covered with sensors and wires tracking my unstable heart rate, part of me was in disbelief that I was back in the hospital. I thought I was doing everything right to heal—eating healthy, taking supplements and exercising. Still, I found myself having a hard time coming to grips with my third hospitalization since being in remission. I knew it was where I needed to be, but I was feeling low and discouraged. My heart ached to be home with my family. It was hard not to be angry. I thought should be at a pumpkin patch enjoying this beautiful fall weather, instead of stuck in the hospital watching the leaves turn beautiful shades of red and orange from my hospital bed. Thoughts like this circled endlessly in my head while my trusty chest port provided easy access for the IV antibiotics to hopefully work their magic and cure my chest infection so I could return home to my family.
After a cancer diagnosis, many patients wait anxiously to hear the words “no evidence of disease. However, cancer survivors often say that life after cancer is where the real journey begins. Once you reach remission it is often difficult to come to grips with all that your body has endured during treatment, both physically and emotionally. Sure, your treatment has ended, and you’ve been told you’re in remission. You’re ready to move on with life after cancer but side effects from treatment may interfere with your quality of life.
Although we may be “cancer-free” we still struggle daily with the side effects of our treatment—chemo brain, neuropathy, pain, weight gain/loss and the fear of reoccurrence. According to the Mayo Clinic, late effects of cancer treatment can come from any of the main types of cancer treatment: chemotherapy, hormone therapy, radiation, surgery, targeted therapy and immunotherapy. The late-term effects of newer cancer treatment like immunotherapy are unknown at this time; however, doctors may find that these treatments also cause late effects in cancer survivors.
Source: Mayo Clinic
Side effects can happen with any type of treatment for cancer, but everyone’s experience is different. Some people have many side effects. Other people have few or none at all.
If you develop side effects, they can happen any time during, immediately after or a few days or weeks after cancer treatment. Most side effects go away on their own or can be treated, but some side effects may last a long time or become permanent.
Side effects of cancer treatment will depend mainly on the type of treatment, the doses used, and if you are getting more than one treatment. Some side effects aren’t always obvious. Your healthcare team might not know that you find it hard to sleep or that you’re having trouble remembering things. Tell them about any side effects that you think are caused by your treatment and how you feel about them. The sooner you tell them of any problems, the sooner your healthcare team can help you cope with them.
Moving Forward Despite the Uncertainty
So much of the cancer journey is uncontrollable and unpredictable. As hard as cancer survivorship can be at times, I’ve found the best way to counteract the side-effects is through self-care and mindfulness.
Our minds are incredibly powerful. Even if something is very small, you can make it into a massive issue in your life by choosing to intensely focus your thoughts upon it. So, I do my best to focus on what I want to make bigger, and not on what I want to avoid. I can’t help what happened and I can’t control what my future will be. But I can be very present and focus on amplifying the good in my life.
One way I try to stay present is mindful is by practicing daily gratitude. Sure, I may experience crippling side-effects at times which make it easy to get lost in all that is going wrong in my life; but if I pause long enough, I can see there are way more things that are going right. And most importantly, I am still here to experience it all—the good and the bad and that is truly a blessing.
Sources:
Cancer survivors: Late effects of cancer treatment. -Mayo Clinic
Late and Long-term Side Effects of Hodgkin Lymphoma Treatment- American Cancer Society
Coping with treatment side effects- Canadian Cancer Society